Yeast infections and Pelvic Inflammatory Disease (PID) are two different health issues. They both affect women’s reproductive health but have nothing to do with each other. Yeast infections come from a fungus called Candida and cause discomfort in the vaginal area.
PID, on the other hand, is often caused by infections spread through sex. If not treated, it can lead to serious problems like infertility. It’s important to know the difference between these two conditions for the right treatment and prevention.
Key Takeaways
- Yeast infections and PID are both significant but unrelated conditions.
- Understanding their differences is crucial for treatment.
- Yeast infections are primarily caused by Candida species.
- PID can lead to severe complications, including infertility.
- Both conditions require different management strategies and prevention approaches.
Understanding Vaginal Infections
Vaginal infections are various conditions that affect the health of the vagina. They can come from both infections and non-infections. It’s key to know about them for treatment and prevention.
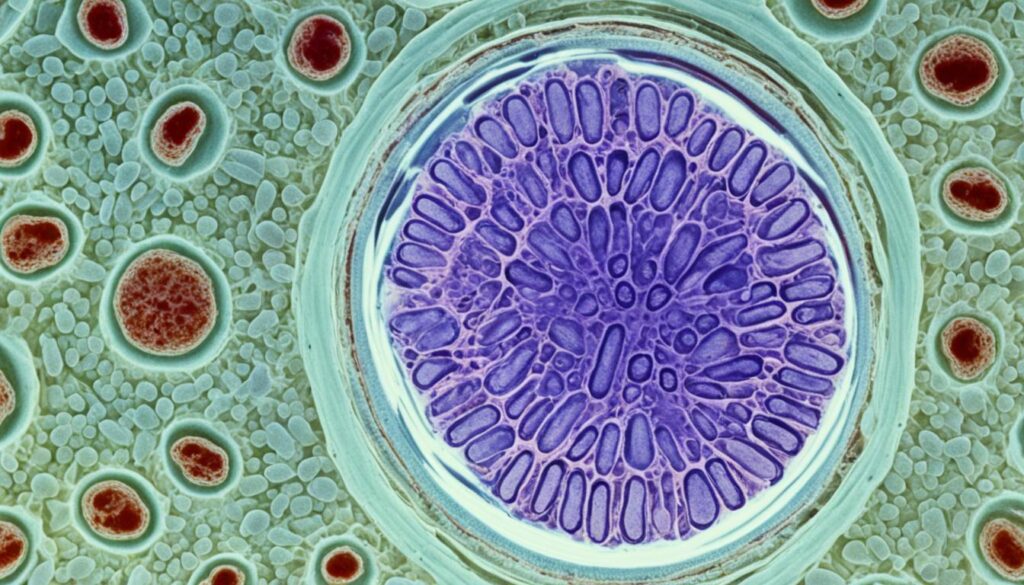
Types of infections include yeast infections, which are very common. These infections are often caused by Candida albicans, a yeast that’s behind most cases.
Bacterial vaginosis is another type, happening when good bacteria in the vagina decrease. Gardnerella bacteria is often found in this condition, causing an imbalance that leads to symptoms.
Trichomoniasis is a sexually transmitted infection. It’s important for women under 26 who are active to get tested for chlamydia. Chlamydia can also cause vaginal inflammation. Other infections like gonorrhea can lead to vaginal discharge and discomfort.
Noninfectious vaginitis can cause irritation from scented products or hormonal changes, especially during menopause. Atrophic vaginitis is a condition seen during menopause. Chronic conditions like vulvodynia show the need to understand vaginal health well.
In summary, understanding vaginal infections means knowing their types and causes. With the right knowledge and care, we can keep our vaginas healthy. For more info, read this detailed article on panic attacks.
What Are Yeast Infections?
Yeast infections are a common type of fungal infection that many women get. It’s important to know the symptoms of yeast infections and why they happen. These infections come from too much Candida fungus in the vagina.
Causes of Yeast Infections
Many things can cause yeast infections. Some reasons include:
- Antibiotics can mess with the balance of bacteria in the body.
- A weak immune system can’t fight off fungal growth well.
- Hormonal changes during pregnancy or when you’re on your period can cause it.
- Diabetes that’s not controlled makes it easy for yeast to grow.
These factors can lead to yeast infections. It’s key to notice any health or lifestyle changes that might cause them.
Common Symptoms of Yeast Infections
Knowing the symptoms of yeast infections is crucial for getting help fast. Look out for:
- A thick, white discharge that looks like cottage cheese
- Itching and irritation around the vagina
- Burning when you pee or have sex
- Redness, irritation, or swelling of the vagina or vulva
These signs can be like other health issues, like bacterial vaginosis or STIs. Always see a healthcare provider to get the right diagnosis and treatment.
What Is Pelvic Inflammatory Disease (PID)?
Pelvic Inflammatory Disease (PID) is a serious health issue that affects a woman’s reproductive health. It happens when an infection spreads to the uterus, ovaries, and fallopian tubes. Often, it comes from not treating sexually transmitted infections like chlamydia and gonorrhea.
Causes of PID
Knowing what causes PID helps in preventing it and treating it early. The main causes are:
- Untreated sexually transmitted infections, especially chlamydia and gonorrhea.
- Having many sexual partners increases the risk of getting an infection.
- Having partners with many sexual partners also raises the risk.
- Douching can change the natural balance of bacteria in the vagina and move bacteria up into the reproductive organs.
- Using an intrauterine device (IUD) can increase the risk during insertion if not tested for STIs first.
Symptoms of Pelvic Inflammatory Disease
Knowing the symptoms of PID helps in getting medical help quickly. Some women may not show any symptoms. But others might have:
- Lower abdominal pain or discomfort.
- Irregular menstrual bleeding.
- Pain during sex.
- Unusual vaginal discharge.
- Fever and chills, which mean a more serious infection.
Getting treatment quickly is key to avoiding serious problems like infertility and chronic pelvic pain. PID affects over 1 million women in the U.S. each year, with about 275,000 needing hospital care. Knowing about What Is Pelvic Inflammatory Disease helps prevent its bad effects.
Yeast Infections and Pelvic Inflammatory Disease: Unrelated
Yeast infections and Pelvic Inflammatory Disease (PID) are two different health issues that affect the vagina. They come from different causes and have different symptoms. Yeast infections happen when too much fungus, like Candida, grows, causing discomfort and discharge. PID, on the other hand, is caused by bacteria in the reproductive organs and can lead to serious problems.
Having pain in the lower abdomen and vaginal discharge can be due to many things. Yeast infections might cause some of these symptoms, but they are not related to PID’s complications. Other conditions like bacterial vaginosis, human papillomavirus infection, or even ectopic pregnancy can also cause these symptoms. This shows why it’s important to know the difference between these unrelated conditions.
If you have pain or discharge that doesn’t go away, you should see a doctor right away. It’s crucial to know the difference between yeast infections and PID because the right treatment depends on it. Making changes to your diet, like eating an anti-inflammatory diet, can also help with chronic fatigue and overall health. For more tips on diet for fatigue relief, check out this useful resource.
Knowing the differences between yeast infections and PID helps people get the right medical care quickly. This can prevent problems linked to these unrelated conditions.
Risk Factors for Yeast Infections
Some things make it more likely to get yeast infections. Knowing these risk factors helps in preventing them. Antibiotics can upset the balance of good bacteria in the vagina, letting yeast grow. Hormonal changes, like during pregnancy or with birth control, also raise the risk.
Diabetes that is not controlled is another big risk. It makes it easier for yeast to grow. People with weaker immune systems, from illness or medicine, are more likely to get yeast infections too.
Knowing these risks helps women watch for symptoms and take steps to prevent yeast infections.
| Risk Factor | Details |
|---|---|
| Recent Antibiotic Use | Disrupts normal vaginal flora balance. |
| Hormonal Fluctuations | Includes changes during pregnancy and high-estrogen contraceptives. |
| Uncontrolled Diabetes | Elevated sugar levels create a conducive environment for yeast. |
| Immunosuppression | Weak immune responses increase susceptibility to infections. |
Diagnosis of Yeast Infections
Health care providers use a careful method to diagnose yeast infections. They need to tell them apart from other conditions with similar symptoms. Getting the diagnosis right is key for the right treatment and care.
How Health Care Providers Diagnose Yeast Infections
The first step in diagnosing yeast infections is a detailed medical history and physical check-up. Providers ask about symptoms, past infections, and any medicines taken. They also use lab tests to help make a diagnosis.
For example, they might take swabs from the vaginal discharge. These are then examined under a microscope. This helps identify Candida species, like Candida albicans, which is the main cause of yeast infections.
About one-third of all vaginitis cases are due to vulvovaginal candidiasis (VVC). It’s important to tell these infections apart from bacterial vaginosis and trichomoniasis. The FDA has recorded 145 studies on vaginitis as of early 2021. Providers use tests that meet strict standards for accurate results.
Testing the vaginal fluid for sialidase activity is key in diagnosing bacterial vaginosis. Tests that can detect different types of vaginitis are also seen as necessary. For people with recurring yeast infections, doctors may suggest special treatments.
| Type of Infection | Common Causing Agent | Symptoms | Diagnosis Method |
|---|---|---|---|
| Vulvovaginal Candidiasis | Candida albicans (90% cases) | Itching, discharge, irritation | Microscopic examination of discharge |
| Bacterial Vaginosis | Various (most common) | Odorous discharge, irritation | Sialidase activity measurement |
| Trichomoniasis | Trichomonas vaginalis | Itching, burning, foul-smelling discharge | NAAT panel testing |
Diagnosis of Pelvic Inflammatory Disease
Diagnosing Pelvic Inflammatory Disease (PID) involves several steps. Healthcare professionals use clinical evaluations and tests to confirm the disease and its severity. It’s important to know the tests used for PID to get the right treatment.
Common Diagnostic Tests for PID
Doctors use a mix of tests to diagnose pelvic inflammatory disease. Here are some key tests:
- Cervical Swab Testing: This test finds bacterial infections that can cause PID.
- Pelvic Examination: A detailed pelvic exam checks for infection signs and tenderness.
- Blood Tests: These check overall health and look for infection markers.
- Imaging Studies: Ultrasounds help see reproductive organs and find any issues.
These tests are crucial for a full Diagnosis of Pelvic Inflammatory Disease. Catching it early means better treatment and outcomes.
Learn how nutrition affects health by checking out this guide. It offers tips on eating for better health.
Treatment for Yeast Infections
Treatment for yeast infections often combines home remedies and medical treatments. Many options are available to help those affected by symptoms like itching, discomfort, and abnormal discharge.
Effective Home Remedies
Home remedies can be very helpful for many women. Some options include:
- Probiotics: Foods like yogurt with live cultures can help balance the vaginal flora.
- Dietary changes: Cutting down on sugar can slow yeast growth.
- Hygiene practices: Keeping the genital area clean and dry lowers infection risk.
While these steps can be useful, severe or recurring infections might need more extensive treatment.
Medical Treatments Available
Medical treatments for yeast infections include antifungal medications. These are very effective. Common treatments are:
| Product Name | Type | Active Ingredient | Duration |
|---|---|---|---|
| Vagistat-1 Ointment | One-day treatment | 6.5% tioconazole | 1 Day |
| Monistat 1-Day Treatment | One-day treatment | 6.5% tioconazole | 1 Day |
| Gyne-Lotrimin 3 Vaginal Cream | Three-day treatment | 2% clotrimazole | 3 Days |
| Vagistat-3 Combination Pack | Three-day treatment | 2% miconazole | 3 Days |
| Gyne-Lotrimin 7 Cream | Seven-day treatment | 1% clotrimazole | 7 Days |
| Monistat 7 Combination Pack | Seven-day treatment | 2% miconazole cream | 7 Days |
Imidazoles cure 85% to 90% of yeast infections. Seeing a healthcare provider is key for proper diagnosis and treatment. This is especially true for ongoing symptoms after using antifungal products.
Treatment for Pelvic Inflammatory Disease
Pelvic inflammatory disease (PID) needs quick and effective treatment to avoid long-term health problems. The main way to handle this is by starting the right treatment for Pelvic Inflammatory Disease. This usually means using broad-spectrum antibiotics to kill the infection and ease symptoms.
Antibiotics and Other Treatments
Studies show antibiotics are key in treating PID, with different types for different infection levels. Here’s a quick look at how well treatments work based on recent studies:
| Medication | Mild-Moderate PID Cure Rate | Severe PID Cure Rate | Adverse Effects Leading to Discontinuation |
|---|---|---|---|
| Azithromycin | RR 1.18 (95% CI 0.89 to 1.55) | RR 1.00 (95% CI 0.96 to 1.05) | RR 0.71 (95% CI 0.38 to 1.34) |
| Quinolones | RR 1.05 (95% CI 0.98 to 1.14) | RR 1.06 (95% CI 0.91 to 1.23) | RR 2.24 (95% CI 0.52 to 9.72) |
| Nitroimidazoles | RR 1.02 (95% CI 0.95 to 1.09) | RR 0.96 (95% CI 0.92 to 1.01) | RR 1.05 (95% CI 0.69 to 1.61) |
In serious cases, hospital care is needed. This is true for severe illness or if complications like abscesses happen. Surgery might also be required for chronic pelvic pain from PID. It’s vital to finish all antibiotics given to prevent the infection from coming back.
With over 750,000 cases a year in the U.S., PID is a big health issue. Health care providers must focus on managing PID well to lower the risk of infertility, which affects about 15% of women with PID. For more on mental health issues linked to physical health, check out the differences between panic and anxiety attacks.
Long-Term Complications of PID
Pelvic Inflammatory Disease (PID) can lead to serious long-term health issues. If not treated or if it comes back, the risks are high. Infertility is a big concern, making it hard for women to have children after PID.
Many women suffer from chronic pelvic pain. This pain can make everyday tasks hard and lower their quality of life. Ectopic pregnancies are also a big risk, where the fertilized egg grows outside the uterus, causing serious problems.
PID can cause the growth of pelvic adhesions. These scar tissues can block the fallopian tubes, making reproductive health issues worse. Women with PID history should get regular check-ups. These visits help monitor their health and can prevent the Long-Term Complications of PID.

| Long-Term Complications | Description | Impact |
|---|---|---|
| Infertility | Inability to conceive after PID | Emotional stress and relationship strain |
| Chronic Pelvic Pain | Persistent pain in the pelvic region | Reduced quality of life |
| Ectopic Pregnancy | Pregnancy occurring outside the uterus | Life-threatening conditions |
| Pelvic Adhesions | Scar tissue formation leading to organ obstruction | Possible surgical intervention required |
Differences in Symptoms and Treatment Approaches
It’s key to know the Differences in Symptoms between yeast infections and pelvic inflammatory disease (PID). Yeast infections cause itching, abnormal discharge, and irritation. PID, however, brings on abdominal pain, fever, and abnormal bleeding.
The Treatment Approaches for Yeast Infections and PID are quite different. Yeast infections are treated with antifungal meds, which help ease symptoms. PID needs antibiotics because it’s caused by bacteria. If you don’t know these differences, you might get the wrong treatment, making things worse.
Recent studies show how important it is to understand the symptoms of different vaginal infections. For more on anxiety and its effects on health, check out the impact of anxiety on health.
Prevention Strategies for Yeast Infections
There are several ways to lower the risk of yeast infections. Keeping the vagina clean is key. Use gentle cleansers and avoid harsh soaps, gels, and bubble baths. Cotton underwear is better than synthetic because it lets air in and keeps the area dry.
What you eat matters too. Eating yogurt with live cultures or taking probiotics can help keep your vagina healthy. This makes it harder for yeast to grow. Knowing about health issues like diabetes or obesity is also important. These can make you more likely to get infections.
It’s important not to use antibiotics when you don’t need them. Antibiotics can mess with the balance of bacteria in your vagina, making yeast infections more likely. Getting tested for STIs like chlamydia and gonorrhea is also key. Catching these infections early can prevent problems later.
By following these tips, you can cut down on yeast infections and keep your vagina healthy.

| Prevention Strategy | Description |
|---|---|
| Vaginal Hygiene | Use gentle, pH-balanced cleansers; avoid harsh soaps and douches. |
| Cotton Underwear | Wearing breathable fabrics helps maintain dryness. |
| Probiotics | Regular consumption of yogurt or supplements fosters healthy flora. |
| Minimize Antibiotic Use | Avoid medications that disrupt normal vaginal flora unless necessary. |
| Health Management | Control underlying conditions like diabetes and obesity. |
| Regular Screenings | Stay updated with STI screenings to avoid complications. |
Conclusion
It’s important for women to know the difference between yeast infections and Pelvic Inflammatory Disease (PID). Both affect vaginal health but need different treatments. Knowing about these conditions helps women take care of themselves.
Being aware is key because not treating these infections can lead to bigger health problems. Yeast infections happen when the vaginal balance is off and can be treated with antifungal meds. PID, linked to STIs, needs antibiotics. Knowing the differences helps women make better health choices.
Women should get medical help to handle these infections. This conclusion highlights the need for quick diagnosis and right treatment. Doing so can prevent long-term health issues from these infections.